Herd immunity won’t stop the outbreak: 3 Dangerous Covid-19 Myths
The spread of misinformation about Covid-19 can only be parallelled by the spread of the virus itself. This would all be in good humour (like the jokes about fighting the virus with alcohol) if it was not so detrimental to many people’s health and mental wellbeing.
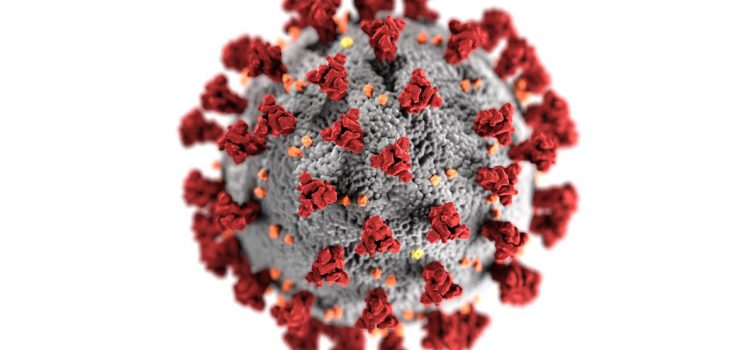
Here at FindMeCure we have always been careful not to present hypotheses as facts and to spread awareness rather than myths and conspiracy theories. Even when the truth is far less compelling. And for sure, some of those myths (like the 5G debacle) are very entertaining but when people’s lives are in danger entertainment is not a priority. Vandalizing cell towers is not going to get rid of this new virus in the corona family and avoiding certain brands of beer is not a good prevention strategy.
Today on the blog we want to dispel the most dangerous Covid-19 myths and conspiracies because the truth is always more complicated. And if the ridiculous is easy to set apart, some of these myths were born out of speculations and theories that are proving to be misleading at best.
Myth 1: The numbers are skewed to control the masses
While many media channels are being unhelpful in this time by presenting a bleaker picture of the situation and feeding into the psychosis brought by this virus, statistics about Covid-19 are not intentionally manipulated.
Whenever there is inaccuracy in numbers it is not with the intention of fear-mongering and control. The far more boring truth is that scientists are not magicians or prophets and estimations cannot always be precise. Although Covid-19 is similar to viruses previously plaguing continents like SARS and MERS, epidemiologists simply don’t have enough information yet to make accurate predictions.
Rates of infection and mortality depend on mass testing which is not currently happening in most places. And even with testing matters are still complicated as not every test is reliable and a false negative can give someone false confidence and lead to further spread.
Your best bet is to rely on trustworthy sources of information. However, keep in mind that it is hard to estimate the rate of mortality if the rate of infection is unknown and in many countries it is.
Myth 2: Herd immunity is the way to go
Herd immunity means that enough people have recovered from the virus and developed immunity to it so that now they cannot infect other people or get sick again themselves. How much is ‘enough’ depends on how contagious a virus is. For example for some diseases like measles, this percentage is very high – 90% of the population needs to be immune to stop the spread. For Covid-19 the herd immunity threshold is 70% but this is only a rough estimate based on the current numbers we’re seeing.
In the case of the coronavirus, however, there are too many unknowns. Firstly, even though scientists are busy developing a vaccine, one is not expected earlier than 2021. This means that in order for herd immunity to work, 50-70% of the world population needs to get infected and then develop antibodies.
Considering the death toll of such a strategy, this is far from the best approach. But another huge question mark here is if it’s even possible for people to become immune for long enough for this theory to even work. For example, if you become immune but this immunity only lasts for a few weeks, this is not long enough to allow for a good proportion of the population to become infected and then immune as well. Thus, herd immunity wouldn’t work in this scenario.
It’s also important to know whether this immunity response is strong enough to prevent re-infection in people who have already had the virus. There are many conflicting reports when it comes to antibodies testing but the truth is that we don’t have a definitive answer yet. Most tests currently available are not reliable and still far too many people have not been tested at all.
That being said, the World Health Organisation reported that only 2-3% of the world population has developed antibodies against the coronavirus. All of this leads to the conclusion that herd immunity is not in the immediate future and we cannot look to it for reassurance.
Myth 3: Healthy young people don’t get sick
Let’s leave aside the implication that young healthy people are the most important segment of the population and everybody else is just a statistic. This kind of thinking is simply not true. It gives young people false confidence and discards cases of serious Covid-19 illness as statistical inevitabilities.
Young, healthy people can and do get seriously ill with Covid-19. In fact, knowing why this happens can be the key to better understanding the disease. There are some theories already – one that states the viral load or in other words, the amount of virus that infects an individual may play the biggest role. Another theory, however, has to do with the response of the immune system.
In some people, like the 47-year-old Joshua Fiske was in great shape before he got infected, the immune system responds disproportionately to the level of risk. The proteins released are called cytokines and the immune response is known as a cytokine storm – it’s so powerful that it can destroy the organism in its intent to protect it.
The process ultimately leads to inflammation and is hard to control because suppressing the immune system leads the organism vulnerable to the virus as well as other infections. On the other hand, not suppressing the immune system can lead to the body’s own immune response destroying it.
Scientists have no way of predicting how a certain organism is going to respond to the virus at this point. The number os seriously ill young, otherwise healthy people, however, indicates that no one is in the clear.
We are not bringing these myths up in order to feed the panic and fear but rather, to educate and prevent that false sense of confidence and security that can lead to not following regulations. So far, social distancing has been successful in slowing down the epidemic. Even if at a certain point we naturally reach herd immunity before a vaccine is developed, it’s better to give researchers that extra time to find antiviral treatments.
If you want to help research advance and speed up the development of Covid-19 treatments, you can join one of the many clinical trials available on our platform. Enter ‘Covid-19′ and start searching.


There are three reasons why herd immunity may not work for India and could also be potentially dangerous—leading to increased hospitalizations that overwhelm the health system and eventually cause a high number of deaths.
First, experts don’t know a lot about COVID-19 immunity, especially how long immunity lasts, what kind of protection it offers, and whether reinfection is possible. These are all questions that researchers around the world, including those at the World Health Organization, are still trying to figure out.
In its cruelest form, pursuing herd immunity without a vaccine is a version of survival of the fittest.
Second, herd immunity is being recommended for India on the assumption that since the country has a large young population (more than 80 percent fall below the age of 44), many of these younger adults will not have a severe reaction to COVID-19.
However, this assumption is problematic as scores of young Indian adults have dangerous underlying conditions and risk factors that could lead to severe complications and death if infected with COVID-19.
Nearly 40 percent of Indian adults aged 45-54 and 22 percent of those aged 20-44 have hypertension; nearly 4 percent of adults aged 15-44 years have reported Type 2 diabetes, along with a high rate of unreported cases; and 2.1 million people are living with HIV, of whom 83 percent are between 15 and 45 years old. Finally, the prevalence of chronic pulmonary disease and asthma among adults was reported as 4.2 and 3 percent, respectively, and nearly a third of adults use tobacco.
With such high rates of comorbidities and risk factors among the young population, letting the virus spread for the sake of an experimental strategy of herd immunity could lead to hundreds of thousands of people being hospitalized and requiring intensive care. Furthermore, seeking herd immunity among younger populations would still require shielding older adults (roughly 50 million Indians are over the age of 65) who are at higher risk.
This raises the question of how to isolate older Indians, many of whom live in multigenerational family homes, which is still the norm—especially in rural parts of the country.
Relying solely on a herd immunity strategy could also be dangerous as it may lower the risk perception among younger populations, affecting their compliance with much-needed social distancing measures.
Third, herd immunity cannot be implemented as a lone strategy. It will still have to be supplemented with ramping up health system capacity, increased cooperation between the public and private health sectors, increased testing, shielding high-risk populations, and implementing gradations of social distancing measures, such as mandatory use of face masks and banning large public gatherings and crowded spaces, which are commonplace in urban India.
I would like to thank you for this amazing article. These myths about coronavirus are very helpful to prevent from COVID-19. Keep sharing awesome posts like this.
You are spreading the dangerous myths Herd immunity is the only way that can stop COVID 19
thank you for standing for truth and disseminating it.